If you missed the town hall, you can watch it on demand. Just click on the UC IT Town Hall link. Dr. Esserman gave a passionate talk about transforming health care – both the business and the outcomes. Here’s a taste of her message:
“A lot of the problem for us in medicine is that physicians and scientists have two blocks… Number one, they don’t really accept that actually medicine and science is a business. It’s actually a big business… And like any other business, we’re driven by the same things that every other business is driven by… We work on exceptional problems… but our businesses are driven a lot by many of the things that drive other businesses. And just like every other business, we’re not like every other business. But that doesn’t mean we can’t adapt some of the tools that have transformed other businesses. The second insight that I’ve had…is the fact that I don’t think people in medicine and science see management as a science. And I think that explains a lot… We think we have to invent it all within medicine. We don’t… Every great idea has been invented someplace else. And the most clever and the best people figure out how to adapt and use tools from one context and apply them in another.”
Photo credit to The Wall Street Journal

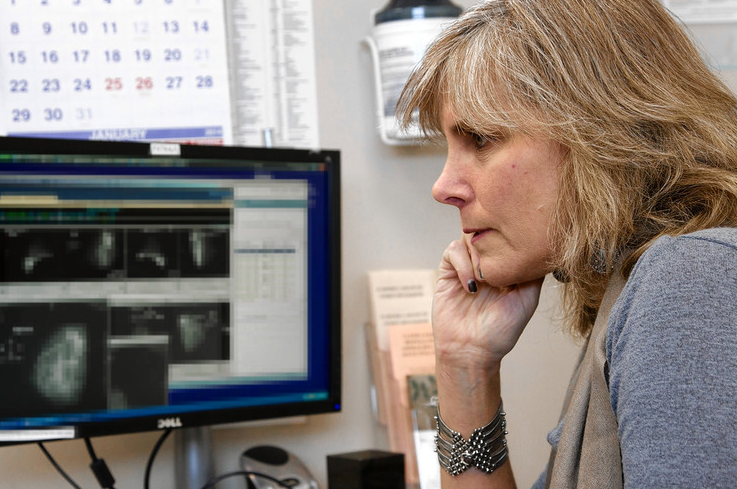




Great presentation Dr. Esserman! I work in healthcare data analytics, and would enjoy hearing what kinds of dashboards, and data metrics you think could bring big improvements to physicians and healthcare. Thanks!
Russ, this is a great question, and we would welcome your input and others’ as well. We are still conducting user interviews, and will be continuously refining our thinking as we learn more; but here are some of the dashboard and data metrics we are currently considering:
DASHBOARDS
For a given patient:
Research Dashboard: shows the patient in real-time what clinical trials s/he is eligible for, and which registries their data was entered into (including what data are missing to be eligible for another trial or registry)
Referral Dashboard: shows what clinical services the patient automatically qualifies for (e.g. smoking cessation, depression interventions, lymphademea prevention) and the real-time status of those referrals, as well as “smart” suggestions of referrals that should be considered
Care Dashboard: shows the overall plan of care for the patient and where s/he is in the journey (a patient-facing dashboard that providers can collaborate on)
For a group of patients:
Population health dashboard: customizable at-a-glance view of a whole practice, a group’s practice, and larger spheres of influence
DATA METRICS
Accuracy Metrics: There is a paucity of accuracy metrics on the extent of errors within Epic or Research databases. There is a sense that the medical records have holes and inconsistencies; we need to identify these so they can be addressed.
Best Practice Metrics: The ultimate quality metric – Clinicians should set quality goals (short/long term) and track patient outcomes and they should measure their practice performance against outside hospitals.
Cost and Value Metrics: Transparency for “spend” on a patients’ care (individually and as a group), what quality are we achieving at that given cost [including specific cost for a given patient: based on their insurance plan, how much is the care plan actually going to cost the patient out of pocket]
Practice Efficiency Metrics: Time, energy, personnel, etc
Population Metrics: The data that allow you to segment the population into high, medium and low risk categories for common diseases we screen for, then apply tailored and proactive care approaches based on the risk category (we do this in our WISDOM study. This could be applied to a variety of conditions like colon cancer, prostate cancer, renal insufficiency, obesity, thyroid cancer, etc)